Backgroud and purpose
In clinical studies in adult acute myeloid leukemia (AML), high ecotropic virus integration-1 (EVI1) gene expression has shown to be an independent prognostic factor. However, the predictive value of high EVI1 expression (EVI1+) in children with AML is little known. The purpose of this study was to investigate frequency and prognostic significance of high EVI1 expression in children with AML.
Patients and methods
Total of 403 newly diagnosed childhood AML patients from 7 centers of south of China from November 2014 to May 2020 were included in the study. A diagnostic assay detecting multiple EVI1 splice variants was developed to determine the relative EVI1 expression by single real-time quantitative polymerase chain reaction in the 403 newly diagnosed pediatirc patients with AML younger than 14 years. Patients were treated with C-HUANAN-AML15 protocol.
In the C-HUANAN-AML15 protocol, tandem 2 courses of FLAG-IDA regimen, or sequential DAE(3+5+10) and DAE(3+5+8) were applied as induction chemotherapy. One course of Homoharringtonine (substitution of Amsacrine in MRC-AML 15 protocol)/ Cytarabine/ Etoposide and one course of Mitoxantrone/ Cytarabine in consolidation chemotherapy were uniform in both groups. 75 patients selected hematopoietic stem cell transplantation (HSCT) in first CR.
The median follow-up period was 20 (0.8 to 67.7) months up to July 2020. The similarity of clinical data was analyzed by the chi square test and COX proportional hazard function model. Complete remission (CR) rates, event-free survival (EFS) and overall survival (OS) were compared by Log-Rank chi square test.
Results
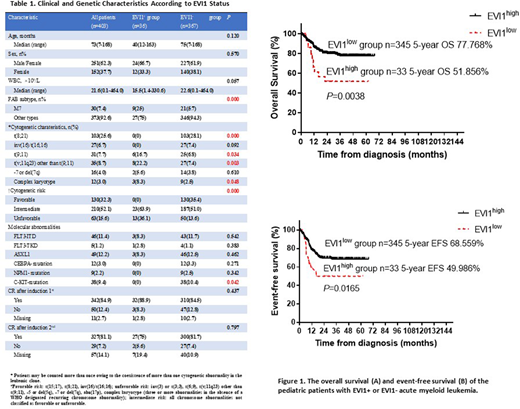
EVI1+ was found in 36/403 (8.9%) of children with de novo AML. The clinical features of the patients with EVI1+(n=36) compared with EVI1-(n=367) AML were summarized in Table 1. No significant differences in sex, white blood cell count, and age were noted between EVI1+and EVI1- AML. When studying the relationship between EVI1+ and conventional classification criteria such as morphology (FAB classification) and cytogenetic data, EVI1+ was predominantly found in FAB M7, t(9;11) and other t(v;11q23), as well as complex karyotype, but mutually exclusive with t(8;21), inv(16)/t(16;16), CEBPA, NPM1 or C-KIT mutations. Furthermore, EVI1+ was significantly associated with unfavoralbe cytogenetic risk. Twenty-five patients (22 cases in the EVI1-group and 3 cases in the EVI1+ group) who gave up treatment or transferred to other hospital when treatment was not completed were excluded, and the remaining 378 AML children with standard treatment were included in the survival analysis. Univariate analysis showed that initial white blood cell count (≥50×109/L), RUNX1-RUNX1T1 fusion gene, FLT3-ITD mutation and EVI1+ affected 5-year EFS (P=0.000, 0.001, 0.016, 0.011). Multivariate prognostic analysis with COX proportional hazard function model for EFS identified EVI1+ as an independent prognosis factor (HR0.531, 95%CI 0.298-0.945, P=0.032). Patients with EVI1+ AML (n=12) who received HSCT in first CR had better 5-year EFS, but the difference was not statistically significant (46.103% vs. 56.250%, P=0.33).
Conclusion
It could be concluded that EVI1+ can be found in ~10% of pediatric AML in China. It is predominantly found in intermediate to unfavorable cytogenetic subtypes and predicts adverse outcome. EVI1 screening at diagnosis should be included in risk stratification of pediatric AML. Whether pediatric patients with EVI1+ AML can benefit from HSCT in first CR needs further reasearch.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.